ZIMBABWE’S junior doctors are on a national strike since the beginning of March protesting against poor remuneration and unsatisfactory working conditions, leading to the closure of almost all central hospitals, children’s units, provincial hospitals and the cessation of emergency life saving procedures throughout the country, according to their representative body, the Zimbabwe Hospital Doctors Association.
According to the association, there are 300 junior doctors working in Zimbabwe’s health government institutions. Zimbabwe is a long way from the World Health Organisation’s recommendation of the minimum threshold of 23 doctors, nurses and midwives per 10 000 population. By 2015, Zimbabwe was at 1.6 physicians and 7.2 nurses per every 10 000.
According to the Zimbabwe National Health Strategy (2016-2020), currently every district has at least 2 doctors, every primary health care centre has at least 2 qualified nurses, 59% of administrative wards are serviced by an Environmental Health Technician and 60% of villages have access to a village health worker.
The Zimbabwe Service Availability and Readiness Assessment Report of 2015 says that health studies and surveys that have been carried out in the country all point towards inadequacies in the six World Health Organization (WHO) Health System Building Blocks – human resources, medical products, vaccines and technology including infrastructure, health financing, health information, service delivery, leadership and governance – that are prerequisites for a functional health delivery system.
What is the status of Zimbabwe’s health delivery system?
At a glance
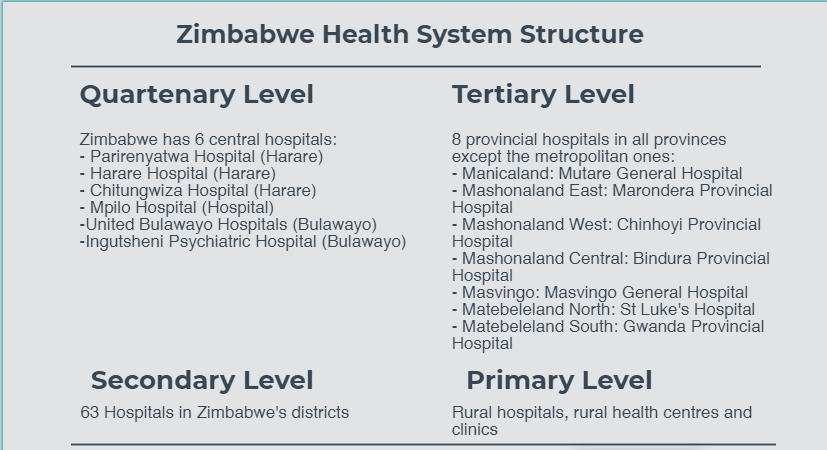
Zimbabwe has a population of 13 061 239 (2012 Census). The total fertility rate is estimated at 4.3 children per woman (15-49years), with the population growth rate estimated at 2.7% per year (source: National Health Strategy for Zimbabwe 2016 -2020 – NHS). The population is served by hospitals and primary health care facilities owned by government (inclusive of security sector – army, police and prisons health care centres), missions, private players and industry. The majority of the population is serviced by government, municipalities and mission care centres.
68% of the health care delivery in the rural areas is from mission hospitals and clinics. Nationally, the mission hospitals and clinics account for 35% of health care delivery. Of these, 22 mission hospitals have been designated district hospitals (source: www.zach.org.zw).
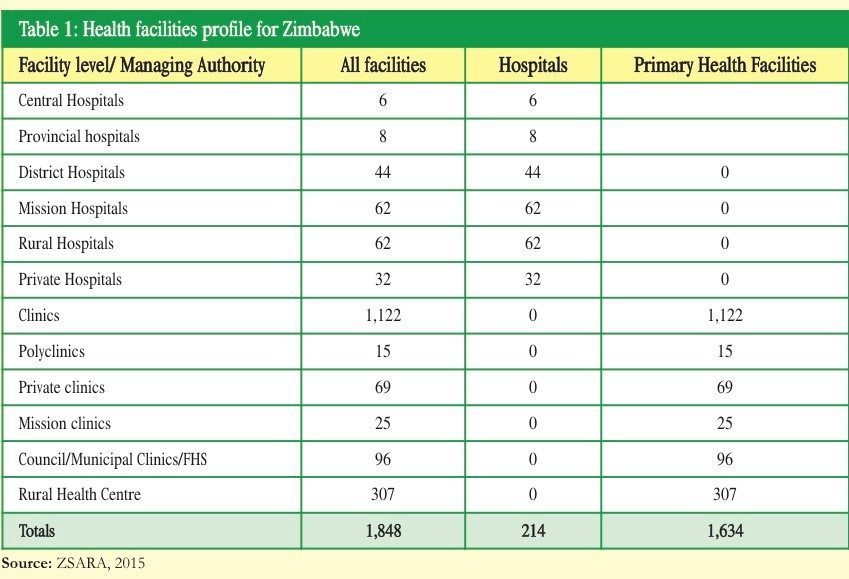
In Zimbabwe, 14% of the health facilities are located in urban areas while 86% are in rural areas. As of 2015, Zimbabwe had 1848 hospitals and primary health care facilities (NHS).
Life expectancy for men has increased from 34.4 in 2006 to 58.5 years in 2013, with women at 61.3 years (WHO, 2013).
Structure
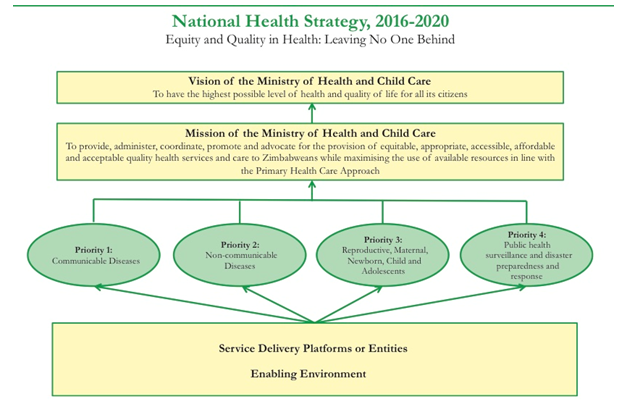
The Health delivery system in Zimbabwe falls under the Ministry of Health and Child Care, with a budget allocation of $520 million for the 2018 financial year. The initial allocation had been $454 million and was increased after Members of Parliament in the National Assembly refused to pass the whole budget unless the allocation was increased.
Legislation
The Zimbabwe health delivery system is built on the constitutional right to health care in Section 76, sub-section 1-4, of the Zimbabwe Constitution, which states that:
- Every citizen and permanent resident of Zimbabwe has the right to have access to basic health care services, including reproductive health
- Every person living with a chronic illness has the right to have access to basic healthcare services for the illness
- No person may be refused emergency medical treatment in any healthcare institution and
- The state must be take reasonable legislative and other measures within the limits of the resources available to it, to achieve the progressive realisation of the rights set out in this section.
The ministry also has a national health strategy in place for the years 2016-2020.
The Ministry itself administers several Acts as follows:
- Anatomical Donations and Post-Mortem Examinations Act
- Atmospheric Pollution Prevention Act
- Concealment of Birth Act
- Dangerous Drugs Act
- Examinations Act
- Food and Food Standards Act
- Government Medical Stores (Commercialisation) Act
- Hazardous Substances and Articles Act
- Health Professions Act
- Health Services Act
- Medical Services Act
- Medicines and Allied Substances Control Act
- Mental Health Act
- National AIDS Council of Zimbabwe Act
- Natural Therapists Act
- Psychological Practices Act
- Public Health Act
- Termination of Pregnancy Act
- Traditional Medical Practitioners Act
- Zimbabwe National Family Planning Council Act

Statistics at a Glance
Malaria incidence – 20 /1000
Maternal mortality rate – 614/100 000
Neonatal mortality rate – 29/1000
Under 5 mortality rate – 75/1000
Proportion of children under 5 stunted – 28%
HIV prevalence (15-49 years) – 14%
TB incidence – 269/100 000
Diabetes prevalence – 10%
Percentage of household members using improved sources of drinking water – 76.1%
Percentage of household members using improved sanitation facilities which are not shared – 35%
Percentage of household members with no facility –31.7%

Did You Know?
- Any person over the age of 18 in Zimbabwe may apply for an order to have you declared mentally disordered or intellectually handicapped.
Section 4 (Application for Reception Order) of the Mental Health Act states that;
- Subject to this Part, an application for a reception order in respect of a person who is believed to be mentally disordered or intellectually handicapped shall be made in the prescribed form by a close relative of the patient or by any other person who has attained the age of eighteen years.
- In an application in terms of subsection (1), the applicant shall state –
- That he believes the patient is mentally disordered or intellectually handicapped; and
- The grounds on which he believes the patient is mentally disordered or intellectually handicapped; and
- The degree of consanguinity or affinity in which the applicant is related to the patient and if he is not a close relative, the reason why the application is made by him instead of by a close relative; and
- That the applicant has personally seen the patient within the seven days preceding the day on which the application was signed.
- An application in terms of subsection (1) shall be made or sent to the magistrate not more than seven days after the day on which it was signed.
- All statements in connection with an application in terms of subsection (1) shall be verified by the affidavit or affirmation of the applicant.
- It is illegal for anyone to advertise sex enhancements products
Section 56 (Publication of advertisements of cures) of the Public Health Act states that;
- No person shall publish any advertisement or statement intended to promote the sale of any medicine, appliance or article for the alleviation or cure of any sexually transmitted disease or disease affecting the generative organs or functions, or of sexual impotence, or of any complaint or infirmity arising from or relating to sexual intercourse.
- Any person who publishes any such advertisement or statement by printing it in any newspaper or exhibiting it to public view in any place or delivering or offering or exhibiting it to any person in any street or public place or in any public conveyance, or who sells offers or shows it or sends it by post to any person, shall be guilty of an offence and liable to a fine not exceeding level four or to imprisonment for a period not exceeding three months or to both such fine and such imprisonment. For the purposes of this section, ‘advertisement’ or ‘statement’ includes any paper, document or book containing any such advertisement or statement.
- This section shall not apply to publications by the Ministry or by any local authority, public hospital or other public body in the discharge of its lawful duties, or by any society or person acting with the authority of the Minister first obtained, or to any books, documents or papers published in good faith for the advancement of medical science.
Factsheet compiled by Lifaqane Nare
Do you want to use our content? Click Here